The Beginning And The End Of Discogenic Pain
Intervertebral disc pathology is one of the primary causes of back and neck pain. The discs are prone to degeneration and injury as they are compressed and twisted through daily activities.
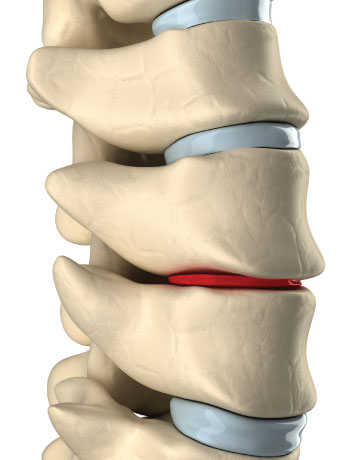
As the disc degenerates, the gel-like nucleus loses its hydration, reducing disc height and creating the possibility of facet syndrome and lateral foraminal stenosis. Furthermore, disc degeneration causes the pliable outer coating of the anulus to become brittle and susceptible to cracks and tears that can lead to disc herniations. Bulging or herniated discs often press on spinal nerves, causing severe pain and radiculopathy.
Damaged intervertebral discs seldom heal because they remain under constant pressure, even while a person is at rest. It is widely accepted that the ideal environment to improve disc pathology is to decompress, or reduce the intradiscal pressures of the damaged disc.
The goal of reducing intradiscal pressure is to enhance the osmotic diffusion of fluids and nutrients across the endplates into the disc, furthering the body’s natural healing abilities. Additionally, reduction of intradiscal pressures may help draw the nucleus pulposus of a herniated disc back into the center, thereby relieving pressure on a compressed nerve root—alleviating the problem and the pain.